Five years… FIVE YEARS! Yesterday Jody celebrated FIVE YEARS since his transplant (insert celebration emoji’s here)! Since the day of his surgery I couldn’t wait for him to hit this big milestone. I can still remember, as if it were yesterday, sitting across from a doctor at the hospital while he told us it was time for Jody to list for new lungs. This would not be without risks, he said, and it wasn’t a cure. The average transplanted lung lasts only five years he said, and only 50% of patients live five years out a double lung transplant. Those statistics were so daunting. As each year passed we celebrated the milestone and I secretly counted down the years until he would reach five years post.
Having reached the five year mark is no guarantee for another year but my understanding is that it generally means less chance of rejection and overall longer survival rates. The significance of decreased rejection risk is that Jody’s doctors might be able to lower his immunosuppression drugs. While these meds are necessary and have worked well for him, they come with big side effects. It’s as if they are aging his body on the inside. While not everything he deals with can be pinpointed to his meds, it seems the answer he hears most frequently from doctors is that it’s related either to his Cystic Fibrosis (which he still has, just not in his lungs) or the transplant drugs. Some of the issues he has had and/or continues to have are:
- Kidney stones (his CF causes him to make stones at a remarkable rate; During his last surgery they blasted 12 stones and the doctors were amazed).
- Gout (he now takes daily meds to help with this but he often experiences flair ups)
- Fragile bones (he broke his wrist bone as a result of this)
- Migraines and daily headaches (with a questionable history of seizure/brain injury on his MRI, he now takes meds to prevent both migraines and seizures).
- Pinched nerve (it took three local ER visits, one hospitalization and a slue of tests to rule out heart/lung issues for this to be diagnosed).
- Hand, feet and thoracic cramps (the thoracic cramps are painful to watch)
- Hand shakes (they never stop moving)
- Bruises easily (he barley touches something and a big bruise appears)
- Memory loss
- Hair loss
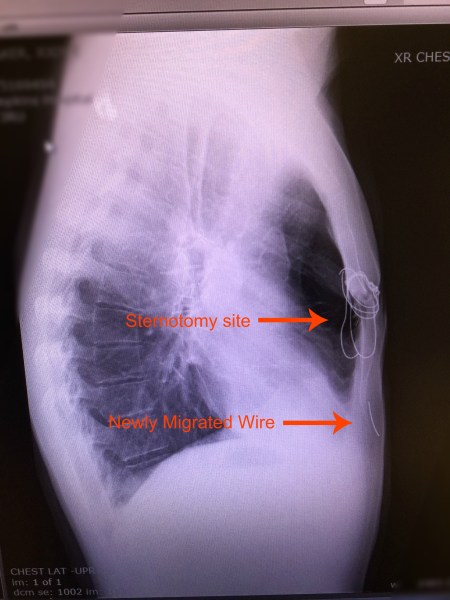
The list could go on and on. He’s had numerous ER visits and surgeries/procedures since his transplant. Remember the broken sternal wires he had to have removed? The bronchoscopy that caused a collapsed lung and need for chest tube and hospitalization? We know another surgery to remove more kidney stones is in his future. Despite all these things, Jody would say post transplant life is pretty good. If you’ve followed Jody’s story you know he’s not a complainer. He accepts his “issues” and doesn’t let them stop him; they pale in comparison to the issues his old CF lungs caused him.
Recently I was listening to the radio in the car and a singer was interviewed and talked about seeing the beauty in hard times. It made me reflect on the hard time we experienced. While in that season of life, fearfully watching Jody’s decline, so. many. hospitalizations., and when the demands of care giving, parenting and work seemed overwhelming, it certainly wasn’t easy for me to ‘see the beauty.’ I couldn’t then… but I can now.
I now see the beauty in the timing of the decline in Jody’s health and need for transplant. While it was really hard to manage everything when our children were so young and we needed lots of help with childcare, our girls are now active in school and sports and we can be involved too. Our oldest daughter swims competitively 11 months of the year and neither Jody nor I have ever had to miss a swim meet because of a hospitalization. When our girls need help with homework, we can give it freely. I cannot imagine how difficult it would be to juggle our life today if Jody were sick and living in and out of the hospital. Our daughters barely remember life when Jody was sick and this, in and of itself, is beautiful.
I now see the beauty in the decline. I can’t imagine saying that five years ago. It was so hard to watch. I hated seeing Jody tied down by oxygen tubing. Listening to his struggle to breathe was heartbreaking. It was sad to see him give up the things he loves: woodworking, yard work, volleyball, etc. But… without the decline there would be no transplant. Without the transplant he wouldn’t have the freedom he has today. He’s back to doing all of those things above and so much more. Before Jody got sick his lung function averaged around 50%, and he did all those activities despite it. Sure, he had lots of coughing and got winded quicker than most people, but he was okay with 50%, it was all he really knew (FYI at time of transplant his lung function was 21%). Today Jody’s lung function is over 100%! If it wasn’t for the decline we would have held onto that 50% with a tight grip but look what happened when we were forced to let go.
I now see the beauty in God’s people. This was pretty easy to see while in the thick of it, but looking back I can better see the magnitude of blessings. People were so generous to us when we needed it most. That generosity came in the form of fundraisers, practical gifts, pick-me-up gifts, acts of service, words of encouragement, prayer and monetary gifts. Friends, family, acquaintances and even strangers stepped up to support us in incredible ways. It’s humbling and we are deeply grateful.
I now see the beauty in the place. How fortunate we were that Jody was able to receive (and continue to receive) his care from one of the best hospitals in the country. This wasn’t always the case. When we were discouraged by his care and sought out the CF clinic at Johns Hopkins, it was closed to us (they, ‘couldn’t accept everyone,’ we were told, there just wasn’t room). It was only through a friend who knew a doctor that Jody was accepted into their CF program. This was a game changer. The care was aggressive and research driven. Although it couldn’t prevent the decline in Jody’s health he was a known patient when it came time for transplant (often patients transfer to a transplant hospital just for the transplant itself). I had so much peace of mind knowing he was in a safe place with a team that knew him and was being well cared for, even when I wasn’t there.
I now see the beauty in the lessons. God clearly asked me to chose hope in a time when I felt hopeless. I wish I could say I did it without hesitation but I fought and struggled with it until I finally agreed to try. Beyond the risks of the surgery itself, it was difficult to be hopeful when I heard things like ‘50% chance of living five years.’ In the end, I wish I had trusted more, hoped more. God knew. The success of Jody’s transplant is no surprise to Him. He knew it was only a matter of time until I would be writing this post, celebrating five years of not just living but thriving!
In anticipation of the five year mark we thought about throwing a celebratory party but opted instead for the quietness of a weekend away. We stayed at a simple cabin in the mountains and enjoyed spending time together, uninhibited by disease or illness. Although the last five years have not been without any medical issues, we can’t put into words how deeply thankful we are for how well Jody has done since his transplant. Dare we hope for another good five years? I say, yes!
Happy 5th Breathday Jody!
If like me, you’d like to take a trip down memory lane and see how far Jody has come, click on the link below to watch a video of Jody’s journey. I made this video for the one year celebration and we enjoy watching it every year on the anniversary of his transplant. https://youtu.be/RQQnI3Izo2M



 going fevers. Jody and I both caught her cold (thankfully not the strep); mine was mild and resolved quickly, Jody couldn’t shake his. After a trip to Hopkins for a nasal swab and evaluation he was diagnosed with
going fevers. Jody and I both caught her cold (thankfully not the strep); mine was mild and resolved quickly, Jody couldn’t shake his. After a trip to Hopkins for a nasal swab and evaluation he was diagnosed with  After a trip to the pediatrician’s office we were reassured that it was just a viral infection that needed to run it’s course. Thankfully that was a 24 hour virus and by the next day she was feeling better.
After a trip to the pediatrician’s office we were reassured that it was just a viral infection that needed to run it’s course. Thankfully that was a 24 hour virus and by the next day she was feeling better.